Relevance of Structural and Functional Impairment in the Breast Cancer Survivor Undergoing Chemotherapy
Main Article Content
Abstract
Background: Breast cancer is the condition suffered by the individual mostly due to transformed lifestyle factor. Impairments leads toactivitylimitation and, this shows, participation in daily household tasks is restricted. In various studies it is observed as the functional impairment has led towards the shoulder joint movement restriction, sensory impairment and also the cognitive impairment due to various drugs during chemotherapy that has the effect of central nervous system. The greater the extent of surgery, more the structures are affected leading to structural impairment.
Objectives: To study the prevalence of structures impaired and the function affected in the breast cancer survivors undergoing chemotherapy.
Methods: The functional impairment is monitored with the help of upper extremity function index. As per the extent of difficulty that is mild, moderate and severe. And on the basis of type of surgeries mostly carried as the treatment for breast cancer evaluates the structures affected during surgery that shows the structural impairment.
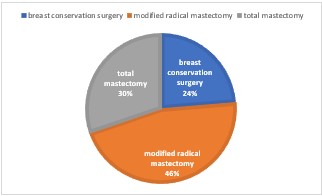
Results: The 76 subjects are included in this study. In which the prevalence of structural impairment is seen on the basis of type of surgery. 46% is seen in modified radical mastectomy and 24% and 30% is in breast conservation surgery and total mastectomy respectively. Where, functional impairment shows prevalence mostly in moderate extent of difficulty that is 78% and mild is observed 17% and severe is only 5%.
Conclusion: The limitations before the surgery were not observed to be affecting the activities of daily living of the patient also decreased ROM, pain like symptoms were noted as not experienced. But later with the surgery and chemotherapy they suffer a lot of difficulties in movements of limb and restricts the range of movement, patient experiences impairments in the function and structure that has impact on daily life. The structural and functional impairments in the patients with breast cancer undergoing the treatment of chemotherapy and prevalence is beheld.
Article Details
References
Bijker R, Duijts SFA, Smith SN, de Wildt-Liesveld R, Anema JR, Regeer BJ. Functional Impairments and Work-Related Outcomes in Breast Cancer Survivors: A Systematic Review. J OccupRehabil. 2018 Sep;28(3):429-451. doi: 10.1007/s10926-017-9736-8. PMID: 29086111; PMCID: PMC6096518
Chaker L, Falla A, van der Lee SJ, Muka T, Imo D, Jaspers L, et al. The global impact of non-communicable diseases on macroeconomic productivity: a systematic review. Eur J Epidemiol. 2015;30(5):357–395
Paalman CH, van Leeuwen FE, Aaronson NK, de Boer AG, van de Poll-Franse L, Oldenburg HS, et al. Employment and social benefits up to 10 years after breast cancer diagnosis: a populationbased study. Br J Cancer. 2016;114(1):81–87.
Yuste Sánchez MJ, Lacomba MT, Sánchez BS, Merino DP, da Costa SP, Téllez EC, Zapico Goñi Á. Health related quality of life improvement in breast cancer patients: secondary outcome from a simple blinded, randomised clinical trial. Breast. 2015 Feb;24(1):75-81. doi: 10.1016/j.breast.2014.11.012. Epub 2014 Dec 10. PMID: 25499599.
Kärki A, Simonen R, Mälkiä E, Selfe J. Impairments, activity limitations and participation restrictions 6 and 12 months after breast cancer operation. J Rehabil Med. 2005 May;37(3):180-8. doi: 10.1080/16501970410024181. PMID: 16040476.
Sahrmann, S. Diagnosis and Treatment of Movement Impairment Syndromes. Mosby Inc; Aug. 200.
Gossenlink R, Rouffaer L, Vanhelden P,Piot W, Troosters T, Christiaens M. Recovery of upper limb function after axillary dissection. J Surg Oncol 2003; 83: 204–211
Gossenlink R, Rouffaer L, Vanhelden P, Piot W, Troosters T, Christiaens M. Recovery of upper limb function after axillary dissection. J Surg Oncol 2003; 83: 204–211
Isaksson G, Feuk B. Morbidity from axillary treatment in breast cancer. A follow-up study in a district hospital. Acta Oncol 2000; 39: 335–336.
Nilsson MI, Olsson M, Wennman-Larsen A, Petersson LM, Alexanderson K. Women’s reflections and actions regarding working after breast cancer surgery—a focus group study. Psychooncology. 2013;22(7):1639–1644.
Tasmuth T. Chronic pain and other symptoms following treatment for breast cancer [dissertation]. Helsinki: University of Helsinki; 1997.
Lash T, Sillman R. Patient characteristics and treatments associated with decline in upper-body function following breast cancer therapy. J Clin Epidemiol 2000; 53: 615–622
World Health Organization. Towards a common language for functioning, disability, and health: ICF. World Health Organization; Geneva, Switzerland: 2002.
Flores AM, Dwyer K. Shoulder impairment before breast cancer surgery. J Womens Health Phys Therap. 2014 Sep;38(3):118-124. doi: 10.1097/JWH.0000000000000020. PMID: 25593563; PMCID: PMC4290873
Xu Z, Luo F, Wang Y, Zou BS, Man Y, Liu JS, Li H, Arshad B, Li H, Li S, Wei YX, Li HY, Wu KN, Kong LQ. Cognitive impairments in breast cancer survivors treated with chemotherapy: a study based on event-related potentials. Cancer ChemotherPharmacol. 2020 Jan;85(1):61-67. doi: 10.1007/s00280-019-03994-0. Epub 2019 Nov 19. PMID: 31745592.
Wefel JS, Saleeba AK, Buzdar AU, Meyers CA. Acute and late onset cognitive dysfunction associated with chemotherapy in women with breast cancer. Cancer. 2010;116(14):3348–56
Chesworth BM, Hamilton CB, Walton DM, Benoit M, Blake TA, Bredy H, Burns C, Chan L, Frey E, Gillies G, Gravelle T, Ho R, Holmes R, Lavallée RL, MacKinnon M, Merchant AJ, Sherman T, Spears K, Yardley D. Reliability and validity of two versions of the upper extremity functional index. Physiother Can. 2014 Summer;66(3):243-53. doi: 10.3138/ptc.2013-45. PMID: 25125777; PMCID: PMC4130402
Gudbergsson SB, Fosså SD, Dahl AA, NOCWO. A study of work changes due to cancer in tumor-free primary-treated cancer patients. A NOCWO study. Support Care Cancer. 2008;16(10):1163–1171.
DiSipio T, Rye S, Newman B, Hayes S. Incidence of unilateral arm lymphoedema after breast cancer: a systematic review and meta-analysis. Lancet Oncol. 2013;14(6):500–515.
Taghian NR, Miller CL, Jammallo LS, O’Toole J, Skolny MN. Lymphedema following breast cancer treatment and impact on quality of life: a review. Crit Rev Oncol Hematol. 2014;92(3):227–234. 17.
Tan FL, Loh SY, Su TT, Veloo VW, Ng L. Return to work in multi-ethnic breast cancer survivors—a qualitative inquiry. Asian Pac J Cancer Prev. 2012;13(11):5791–5797
Loudon L, Petrek J. Lymphedema in women treated for breast cancer. Cancer Pract 2000; 8: 65–71.