Role of Ultrasound Elastography in Characterization of Focal Solid Hepatic Lesion
Main Article Content
Abstract
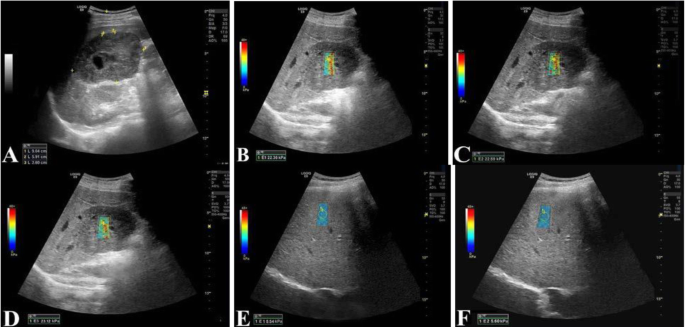
Purpose: Analysis of focal solid hepatic lesions by 2D Shear Wave Sono-Elastography and evaluation of its diagnostic accuracy in differentiating benign from malignant lesions.
Methodology: This study included 58 patients all the studied patients were subjected to grey-scale ultrasound and 2D shear wave sono-elastography which were performed on LOGIQTM P9 XDclearTM (GE Healthcare) ultrasound machine with convex transducer (C1-5-D 3.5 MHz).
Results: Sono-elastography showed that most malignant lesions had higher stiffness (median = 33.4 kPa) and showed mixed colour with red foci, whereas most benign lesions had lower stiffness (median = 13.5 kPa) and showed yellow-green color.
Amongst the malignant lesions, hepatocellular carcinomas showed comparatively lower stiffness values (median = 29.25 kPa) than those of metastases and cholangiocarcinomas (median = 36.65 kPa and 39.3 kPa, respectively), and cholangiocarcinoma was established as the stiffest focal solid hepatic lesion.
Among the benign lesions, focal nodular hyperplasia showed higher stiffness (median = 23.7 kPa). Hemangiomas were comparatively softer lesions; however, they showed higher stiffness values (median = 13.3 kPa) as compared to surrounding normal liver parenchyma (median = 4.45 kPa).
Because of the associated diffuse liver fibrosis, hepatocellular carcinomas had the highest stiffness values of background liver parenchyma (median = 11.1 kPa). This, in turn, resulted in a lower lesion/parenchyma stiffness ratio (median = 2.9) in contrast to other malignant lesions (median = 5.7 and 6.3 for metastases and cholangiocarcinoma’s, respectively), with values similar to those seen in cases of benign lesions (median = 2.8).
The threshold cut off value to differentiate benign from malignant solid focal hepatic lesions based on their SWE characteristics was assigned as 15.9 kPa. Using this value with the AUC of 0.9545, the ROC analysis resulted in 100% sensitivity, 90.91% specificity, 97.92% positive predictive value (PPV), 100% negative predictive value (NPV), and 98.28% accuracy.
Conclusion: This study has demonstrated that 2D shear wave sono-elastography is a robust technique and is capable of evaluating stiffness changes in the liver associated with solid focal liver lesions, which helps in distinguishing benign from malignant lesions and also in their sub-categorization, i.e., differentiating focal nodular hyperplasia from hemangioma and differentiating hepatocellular carcinoma from cholangiocarcinoma and metastases, with high sensitivity and accuracy. Thus, it can be added to routine grey-scale sonographic examinations for rapid, cost-effective, non-invasive, and non-contrast assessments to aid the diagnosis and further management.
Article Details
References
Bruix J, Sherman M. American Association for the Study of Liver. Management of hepatocellular carcinoma: an update. Hepatology 2011;53: 1020 – 2
Khan SA, Davidson BR, Goldin RD et al. Guidelines for the diagnosis and treatment of cholangiocarcinoma: an update. Gut 2012;61: 1657 – 69
European Association for the Study of the Liver; European Organisation for Research and Treatment of Cancer. EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol 2012;56: 908 – 43
Marrero JA, Ahn J, Reddy KR.ACG clinical guideline: the diagnosis and management of focal liver lesions. The American journal of gastroenterology. 2014;109(9):1328
Bastati N, Feier D, Wibmer A et al.Noninvasive differentiation of simple steatosis and steatohepatitis by using gadoxetic acid-enhanced MR imaging in patients with nonalcoholic fatty liver disease: a proof-of-concept study. Radiology2014;271:739–747
Smith-Bindman R, Miglioretti DL, Johnson E et al. Use of diagnostic imaging studies and associated radiation exposure for patients enrolled in large integrated health care systems, 1996-2010. JAMA 2012;9:307–2400
Bosch FX, Ribes J, Cléries R et al. Epidemiology of hepatocellular carcinoma. Clin Liver Dis 2005;9(2):191–211
Ishak KG, Rabin L. Benign tumors of the liver. Med Clin North Am 1975;59 (4):995–1013
Gandolfi L, Leo P, Solmi L, Vitelli E, Verros G, Colecchia A. Natural history of hepatic haemangiomas: clinical and ultrasound study. Gut 1991;32(6):677– 680
Tian WS, Lin MX, Zhou LY et al. Maximum value measured by 2-D shear wave elastography helps in differentiating malignancy from benign focal liver lesions. Ultrasound Med Biol2016;42(9):2156–2166
Bedossa P, Dargere D, Paradis V. Sampling variability of liver fibrosis in chronic hepatitis C. Hepatology 2003;38:1449–1457
Atwell TD, Smith RL, Hesley GK et al. Incidence of bleeding after 15,181 percutaneous biopsies and the role of aspirin. AJR Am J Roentgenol2010;194:784–789
Liana G, Speranta I, Cristian G. Real-time sonoelastography: a new application in the field of liver disease. J Gastrointestin Liver Dis 2008;17(4):469–474
Gutiérrez MV, Enciso RJ. Liver elastography: what it is, how it is done, and how it is interpreted. Radiologia. 2017;60(3):183–189
Fang C, Jaffer OS, Yusuf GT et al. Reducing the number of measurements in liver point shear-wave elastography: factors that influence the number and reliability of measurements in assessment of liver fibrosis in clinical practice. Radiol2018;287(3):844–852
Jeong WK, Lim HK, Lee HK et al. Principles and clinical application of ultrasound elastography for diffuse liver disease. Ultrasonography 2014;33(3):149–160
Ferraioli G, Parekh P, Levitov AB et al. Shear wave elastography for evaluation of liver fibrosis. J Ultrasound Med 2014;33(2):197–203
Samir AE, Dhyani M, Vij A et al. Shear wave elastography for the estimation of liver fibrosis in chronic liver disease: determining accuracy and ideal site for measurement. Radiology 2015;274:888–896
Varbobitis IC, Siakavellas SI, Koutsounas IS et al. Reliability and applicability of two-dimensional shear-wave elastography for the evaluation of liver stiffness. Eur J GastroenterolHepatol2016;10:1204–1209
Guibal A, Boularan C, Bruce M et al. Evaluation of shear wave elastography for the characterization of focal liver lesions on ultrasound. EurRadiol. 2013;23(4):1138–1149
GallottiA, Donofrio M, Romanini L, Cantisani V, PozziMucelli R. Acoustic radiation force impulse (ARFI) ultrasound imaging of solid focal liver lesions. Eur J Radiol 2012;81(3): 451-5.
Abdel-Latif et al. Role of shear wave sono-elastography (SWE) in the characterization of hepatic focal lesions. Egyptian Journal of Radiology and Nuclear Medicine 2020;51:68.
Guibal A, Boularan C, Bruce M et al. Evaluation of shear wave elastography for the characterization of focal liver lesions on ultrasound. EurRadiol. 2013;23(4):1138–1149
Choong KL, Wong YH, Yeong CH et al. Elasticity characterization of liver cancers using shear wave ultrasound elastography: comparison between hepatocellular carcinoma and liver metastasis. Journal of Diagnostic Medical Sonography 2017;33(6):481–488.
Park HS, Kim YJ, Yu MH et al. Shear wave elastography of focal liver lesion: intraobserver reproducibility and elasticity characterization. Ultrasound Q 2015;31:262–271.
Gerber L, Fitting D, Srikantharajah K et al. Evaluation of 2D- shear wave elastography for characterization of focal liver lesions. J Gastrointestin Liver Dis 2017;3:283–290.
Yu H, Wilson SR. Differentiation of benign from malignant liver masses with acoustic radiation force impulse technique. Ultrasound Q 2011;27(4): 217–223
Qiang Lu, Changli Lu, Jiawu LI et al. Hepatocellular carcinoma: stiffness value and ratio to discriminate malignant from benign focal liver lesions. Radiology 2015;275(3):880–888
Sirica AE, Campbell DJ, Dumur CI. Cancer-associated fibroblasts in intrahepatic cholangiocarcinoma. CurrOpin Gastroenterol 2011;27:276–284
Okamoto K, Tajima H, Ohta T et al. Angiotensin II induces tumor progression and fibrosis in intrahepatic cholangiocarcinoma through an interaction with hepatic stellate cells. Int J Oncol 2010;37:1251–1259
Heide R, Strobel D, Bernatik T et al. Characterization of focal liver lesions (FLL) with acoustic radiation force impulse (ARFI) elastometry. Ultraschall Med 2010; 31:405–409
Kim JE, Lee JY, Bae KS et al. Acoustic radiation force impulse elastography for focal hepatic tumors: usefulness for differentiating hemangiomas from malignant tumors. Korean J Radiol2013;14(5):743–753
Frulio N,Laumonier H, Carteret T et al. Evaluation of liver tumors using acoustic radiation force impulse elastography and correlation with histologic data. J Ultrasound Med 2013;32(1):121–130
Gallotti A, D’Onofrio M, Romanini L et al. Acoustic radiation force impulse (ARFI) ultrasound imaging of solid focal liver lesions. Eur J Radiol2012;81(3):451–455
Brunel T, Guibal A, Boularan C et al. Focal nodular hyperplasia and hepatocellular adenoma: the value of shear wave elastography for differential diagnosis. Eur J Radiol2015;84(11):2059–2064
Ferraioli G, Wai-sun IW, Castera L et al. Liver ultrasound elastography: an update to the world federation for ultrasound in medicine and biology guidelines and recommendations. Ultrasound Med Biol 2018;1–22
Xie LT, Yan CH, Zhao QY et al. Quantitative and non-invasive assessment of chronic liver diseases using two-dimensional shear wave elastography. World J Gastroenterol 2018;24(9):957–970.
De-Wall RJ, Bharat S, Varghese T et al. Characterizing the compression-dependent viscoelastic properties of human hepatic pathologies using dynamic compression testing. Phys Med Biol 2012;57(8):2273– 2286.