Assessment of Debriefing Experiences of Emergency Medical Professionals in Remote Simulation and Standardized Patients
Main Article Content
Abstract
INTRODUCTION:
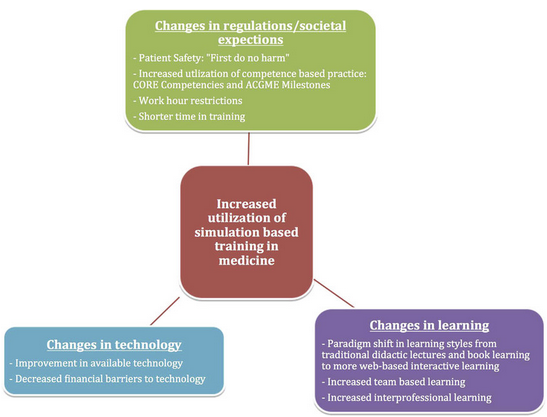
Clinical training of medical students during their formative years of graduation and post-graduation forms the basis of their future clinical practice. Hands-on practice and bed-side teaching form the cornerstones of effective clinical education, but recently the utilization of simulation based medical education, is growing at a fast pace.
Students are exposed to Simulated Clinical Experiences (SCE’s) in a safe and controlled environment. Simulation based training has been found to be a better tool than didactic teaching for medical graduate students to learn critical assessment and life-saving skills.Emergency Medicine requires expert and skilled professionals to handle critical situations with instantaneous decision making in order to save a patient’s life.Reflective debriefing helps learners tackle real life emergencies more effectively.
OBJECTIVE:
To compare debriefing experiences of Emergency Medical Professionals after sessions in remote simulation and standardized patients.
METHODOLOGY:
Only those EMPs who had not been exposed to simulation, debriefing and ITLS sessions in the past participated in the study. The Facilitator demonstrated the skills to the participants and written patient assessment algorithms were distributed for better understanding.
The EMPs were randomly assigned into two groups A and B. Group A was exposed to Standardized Patients (SP) Simulation while Group B was exposed to Remote Manikin Simulation.
CONCLUSION:
Remote Simulation has been largely successful as it is reiterated by the high satisfaction scores in our study. Nevertheless, in-person SP simulation, provided a richer debriefing experience to the learners.
Article Details
References
Guragai M, Mandal D. Five Skills Medical Students Should Have. JNMA J Nepal Med Assoc. 2020 Apr 30;58(224):269-271. doi: 10.31729/jnma.4878. PMID: 32417868; PMCID: PMC7580471.
Qureshi, Zeshan& Maxwell, Simon. (2011). Has bedside teaching had its day? Advances in health sciences education : theory and practice. 17. 301-4. 10.1007/s10459-011-9308-1.
Everson J, Gao A, Roder C, Kinnear J. Impact of Simulation Training on Undergraduate Clinical Decision-making in Emergencies: A Non-blinded, Single-centre, Randomised Pilot Study. Cureus. 2020 Apr 12;12(4):e7650. doi: 10.7759/cureus.7650. PMID: 32411551; PMCID: PMC7217257.
Davis D, Warrington SJ. Simulation Training and Skill Assessment in Emergency Medicine. [Updated 2022 May 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557695/
Steadman RH, Coates WC, Huang YM, Matevosian R, Larmon BR, McCullough L, Ariel D. Simulation-based training is superior to problem-based learning for the acquisition of critical assessment and management skills. Crit Care Med. 2006 Jan;34(1):151-7. doi: 10.1097/01.ccm.0000190619.42013.94. PMID: 16374169.
Pothiawala, Sohil& Lateef, Fatimah. (2012). Simulation Training in Emergency Medicine (STEM): An Integral Component of Residency Curriculum. Hong Kong Journal of Emergency Medicine. 19. 10.1177/102490791201900107.
Grice GR, Wenger P, Brooks N, Berry TM. Comparison of patient simulation methods used in a physical assessment course. Am J Pharm Educ. 2013 May 13;77(4):77. doi: 10.5688/ajpe77477. PMID: 23716745; PMCID: PMC3663631.
Mary Latina Mayville Debriefing: The Essential Step in Simulation, Newborn and Infant Nursing Reviews, Volume 11, Issue 1, 2011, Pages 35-39, ISSN 1527-3369, https://doi.org/10.1053/j.nainr.2010.12.012
Musa D, Gonzalez L, Penney H, Daher S. Interactive Video Simulation for Remote Healthcare Learning. Front Surg. 2021 Aug 10;8:713119. doi: 10.3389/fsurg.2021.713119. PMID: 34447784; PMCID: PMC8384032.
Hanoun, Samer&Nahavandi, Saeid. (2018). Current and future methodologies of after action review in simulation-based training. 1-6. 10.1109/SYSCON.2018.8369516.
Durham CF, Alden KR. Enhancing Patient Safety in Nursing Education Through Patient Simulation. In: Hughes RG, editor. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville (MD): Agency for Healthcare Research and Quality (US); 2008 Apr. Chapter 51. Available from: https://www.ncbi.nlm.nih.gov/books/NBK2628/
M. Patricia Wickers, Establishing the Climate for a Successful Debriefing, Clinical Simulation in Nursing, Volume 6, Issue 3, 2010, Pages e83-e86, ISSN 1876-1399, https://doi.org/10.1016/j.ecns.2009.06.003.
Sawyer TL, Deering S. Adaptation of the US Army's After-Action Review for simulation debriefing in healthcare. Simul Healthc. 2013 Dec;8(6):388-97.
Cheng A, Kolbe M, Grant V, Eller S, Hales R, Symon B, Griswold S, Eppich W. A practical guide to virtual debriefings: communities of inquiry perspective. Adv Simul (Lond). 2020 Aug 12;5:18. doi: 10.1186/s41077-020-00141-1. PMID: 32817805; PMCID: PMC7422458.
Cheng, A., Grant, V., Robinson, T., Catena, H., Lachapelle, K., Kim, J., Adler, M., &Eppich, W. (2016). The Promoting Excellence and Reflective Learning in Simulation (PEARLS) Approach to Health Care Debriefing: A Faculty Development Guide. Clinical Simulation in Nursing, 12(10), 419-428. https://doi.org/10.1016/j.ecns.2016.05.002
Honda R, McCoy CE. Teledebriefing in Medical Simulation. [Updated 2021 Sep 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK546584/
Reed, S. J. (2012). Debriefing experience scale: Development of a tool to evaluate the student learning experience in debriefing. Clinical Simulation in Nursing, 8(6), e211-7.
doi:10.1016/j.ecns.2011.11.002.
Hashem, Somaya, Et Al. "A Simple Multilinear Regression Model For Predicting Fibrosis Scores In Chronic Egyptian Hepatitis C Virus Patients." International Journal Of Bio-Technology And Research 4.3 (2014): 37-46.
Agarwal, P. A. R. U. L. "Review Of Patient Satisfaction In Private Hospitals-A Study Of Health Care Sector With Special Reference To Noida & Ghaziabad." International Journal Of Sales & Marketing Management Research And Development 4.2 (2014): 27-34.
Hanuma, P., Et Al. "Multi-Dimensional Flow Analysis Of Goldberg Falcon Remote Controlled Aircraft Wing." International Journal Of Mechanical And Production Engineering Research And Development (IJMPERD) 8.4: 1-8.
Ahuja, KANIKA K., And T. A. N. I. K. A. Pundir. "No ‘Pretty’please At Work: Studying Effect Of Gender And Physical." International Journal Of Human Resource Management And Research 9.2 (2019): 83-94.
Srivastava, Pooja Raj. "Thematic Considerations Of Displacement And Amitav Ghoshas The Circle Of Reason, The Shadow Lines, The Glass Palace And The Sea Of Poppies." International Journal Of English And Literature (IJEL) 6.1 (2016): 85-96.
Thongnoppakun, W. A. R. A. N. G. K. A. N. A., And C. H. O. K. C. H. A. I. Yuenyong. "Developing Preservice Science Teachers’ Pedagogical Content Knowledge Using Cores-Based Activity." International Journal Of Educational Science And Research 8.4 (2018): 1-8.